Three trials recently published in the NEJM issue last week are rocking the world of nephrology.
These three European Trials come as a major surprise to me.
Two of them deal with the Mtor inhibitors and a clinical trial showing major disappointment in terms of decreasing GFR when used for polycystic kidney disease.
Its not the first time that the basic science data is contradicting clinical data. A nice editorial in NEJM also gives some insightful thoughts on this topic. For now, we have to await some more trails, perhaps longer term to see where we go with this drug.
Another shocker was the IDEAL trial.
This compared early initiation vs late initiation. In this study, planned early initiation of dialysis in patients with stage V chronic kidney disease was not associated with an improvement in survival or clinical outcomes.
This is an interesting study. It compared starting dialysis at 5-7ml/min vs standard practice right now and showed no difference. This goes back to the olden days when people started dialysis when patients got symptomatic rather than just a number. Perhaps we might be just going around in circles.
But some other bloggers have good comments to say.
Take a look
https://www.pediatric-nephrology.com/home/2010/06/29/233-mtoradpkd.html
https://www.pediatric-nephrology.com/home/2010/06/29/232-dialysisckdv.html
http://www.uremicfrost.com/2010/06/does-early-initiation-of-dialysis-help_27.html
http://www.uremicfrost.com/2010/06/early-vs-late-hd-initiation-video.html
http://www.uremicfrost.com/2010/06/does-early-initiation-of-dialysis-help.html
References:
http://www.ncbi.nlm.nih.gov/pubmed/20581422( IDEAL TRIAL)
http://www.ncbi.nlm.nih.gov/pubmed/20581393 ( EDITORIAL NEJM MTOR)
http://www.ncbi.nlm.nih.gov/pubmed/20581392
http://www.ncbi.nlm.nih.gov/pubmed/20581391
Wednesday, June 30, 2010
Monday, June 21, 2010
IN THE NEWS:- Angiotensin-receptor blockade and risk of cancer: meta-analysis of randomised controlled trials.
Experimental studies implicate the role of the renin-angiotensin system, particularly angiotensin II type-1 and type-2 receptors, in the regulation of cell proliferation, angiogenesis, and tumour progression. A meta analysis done and published in Lancet Oncology showed that patients randomly assigned to telmisartan had a significantly increased risk of new cancer occurrence compared with patients in control groups (7.2%vs 6.0%, risk ratio [RR] 1.08, 95% CI 1.01-1.15; p=0.016). Among specific solid organ cancers examined, only new lung-cancer occurrence was significantly higher in patients randomly assigned to receive ARBs than in those assigned to receive control.
This comes with no surprise given this finding was recently also noted in the large trial that showed that the combination of acei and arbs was causing more hyperkalemia and hypotension. It is interesting though that in animal modes, ACEI and ARBS have an anti VEGF effect and here it is showing increased tumor burden and why just lung cancer( given the location of the enzymes perhaps). I gather it has to be due to Anti TGF-B properties or VEGF biology. But I am not sure
More studies of such need to be done before we say this is final and avoid these drugs.
More studies of such need to be done before we say this is final and avoid these drugs.
Some references
Labels:
General Nephrology,
Hypertension,
In The News
Sunday, June 20, 2010
CONSULT ROUNDS: Hypocomplementemia!
C3, C4 is what we usually order.
The classical complement pathway activates C4 as well as C3. This can lead to low C3 and C4 levels which lead to decreased CH 50. This would typically be seen with complement activation driven by immune complexes (lupus, hepatitis C, cryoglobulinemia).
Alternative complement pathway activation is typically driven by bacterial or microbial antigens: C3 is directly activity producing low C3 and decreased CH 50 C4 is normal. C3 may also be directly activated by C3 nephritic factor which is an antibody which activates C3 convertase directly (associated with dense deposit disease).
Diseases which do not have bacterial/microbial antigens or circulating immune complex will typically have normal levels of serum complement and normal CH 50. IgA nephritis does not cause low serum complements as IgA is a poor complement activator. ANCA diseases do not produce circulating immune complexes, for us, complement levels are normal. For unclear reasons, anti-GBM disease typically presents with normal complement levels
Six classical diseases come to mind when one sees low C3 and low C4.
Lupus nephritis
Subacute bacterial endocarditis
MPGN 1 and 2
Post-streptococcal glomerulonephritis
Cryoglobulinemic glomerulonephritis ( usually c4 more than c3)
Atheroembolic renaldisease
HUS/TTP.
The classical complement pathway activates C4 as well as C3. This can lead to low C3 and C4 levels which lead to decreased CH 50. This would typically be seen with complement activation driven by immune complexes (lupus, hepatitis C, cryoglobulinemia).
Alternative complement pathway activation is typically driven by bacterial or microbial antigens: C3 is directly activity producing low C3 and decreased CH 50 C4 is normal. C3 may also be directly activated by C3 nephritic factor which is an antibody which activates C3 convertase directly (associated with dense deposit disease).
Diseases which do not have bacterial/microbial antigens or circulating immune complex will typically have normal levels of serum complement and normal CH 50. IgA nephritis does not cause low serum complements as IgA is a poor complement activator. ANCA diseases do not produce circulating immune complexes, for us, complement levels are normal. For unclear reasons, anti-GBM disease typically presents with normal complement levels
Six classical diseases come to mind when one sees low C3 and low C4.
Lupus nephritis
Subacute bacterial endocarditis
MPGN 1 and 2
Post-streptococcal glomerulonephritis
Cryoglobulinemic glomerulonephritis ( usually c4 more than c3)
Atheroembolic renaldisease
HUS/TTP.
IN THE NEWS ---> Stem Cells and Kidney Damage
A recent case in JASN talks about a new complication seen with stem cell infusion. Please have a look at this news from the BBC website. Stem cells were injected into the kidney, but the patient suffered tissue damage and died from an infection. Perhaps the enthusiasm is still too early. Although the animal studies have shown promise of stem cell therapy in renal disease, in this particular cae, they found that the patient had not benefited at all from the treatment, but had actually developed tissue damage called angiomyeloproliferative lesions at the injection sites. These were found to be clusters of blood vessels and bone marrow cells. What is angiomyeloproliferative lesion: could be a precede cancer. The neoplastic potential, of this lesion is unknown.
More work is needed in this field to clarify these effects.
References:
Labels:
General Nephrology,
glomerular diseases,
In The News
Saturday, June 19, 2010
Answer to Immunology Quiz 2
Immunology Quiz 2:
Which of the following drug & target of action combinations incorrectly matched?
Responses:
Tacrolimus/Calcineurin - 16%
Basiliximab/CD3 - 66%
MMF/IMPDH - 8%
Sirolimus/mTOR - 16%
Belatacept/CD80,86 - 33%
Compath/CD52 - 8%
OKT3/CD25 - 66%
Answer:
As majority of you indicated, the incorrect combinations are Basiliximab/CD3 and OKT3/CD25. Basiliximab acts by blocking IL2 receptor, also known as CD25. OKT3 or Muromonab-CD3 is a monoclonal antibody to CD3 on T cells. 33% of you marked Belatacept/CD80,86 as incorrect combination. However, this is a wrong choice as CD80/86 on antigen presenting cells is indeed the target of action for Belatacept there by inhibiting CD28 costimulation pathway of T cell activation.
Which of the following drug & target of action combinations incorrectly matched?
Responses:
Tacrolimus/Calcineurin - 16%
Basiliximab/CD3 - 66%
MMF/IMPDH - 8%
Sirolimus/mTOR - 16%
Belatacept/CD80,86 - 33%
Compath/CD52 - 8%
OKT3/CD25 - 66%
Answer:
As majority of you indicated, the incorrect combinations are Basiliximab/CD3 and OKT3/CD25. Basiliximab acts by blocking IL2 receptor, also known as CD25. OKT3 or Muromonab-CD3 is a monoclonal antibody to CD3 on T cells. 33% of you marked Belatacept/CD80,86 as incorrect combination. However, this is a wrong choice as CD80/86 on antigen presenting cells is indeed the target of action for Belatacept there by inhibiting CD28 costimulation pathway of T cell activation.
Labels:
immunology,
kidney transplantation,
quiz
Rituximab for induction?
A trial from Sweden was published last year in Transplantation. It was a prospective, double blind, randomized, placebo-controlled multicenter study on the efficacy and safety of rituximab as induction therapy, together with tacrolimus, mycophenolate mofetil, and steroids in kidney transplants. The primary endpoint was defined as acute rejection, graft loss, or death during the first 6 months. They randomized 140 patients and found no difference in rejection episodes, infection episodes. There was a tendency toward fewer and milder rejections during the first 6 months in the rituximab group. A commentary of this also got published in recent May issue of Transplantation.
More trials need to be done with this agent before we think it can be used as an induction agent. Trails of using it as an induction in lupus also have been done in Europe with promising results.
Other areas where it is being used in highly sensitized individuals to desensitize. In cases of historical cross matches that are positive. Rituximab is becoming standard drug to give patients with antibody mediated rejection.
More trials need to be done with this agent before we think it can be used as an induction agent. Trails of using it as an induction in lupus also have been done in Europe with promising results.
Other areas where it is being used in highly sensitized individuals to desensitize. In cases of historical cross matches that are positive. Rituximab is becoming standard drug to give patients with antibody mediated rejection.
Friday, June 18, 2010
TOPIC DISCUSSION: Phosphorous containing foods
We all tell ESRD patients to avoid phos containing foods. Additives to foods also contain a lot of phos that might be missed. A nice tool developed by Case Western helps out physicians and patients. It takes you by the Fast Food Restaurant and tells you how much phos is in each food product and how much in additives.
Not only that, it then gives an option for a better choice to eat. Check it out
http://www.case.edu/med/ccrhd/phosfoods/
Other good references are: ( both are articles by one of Nephronpower bloggers: Ojas Mehta)
http://www.ncbi.nlm.nih.gov/pubmed/19628683
http://www.ncbi.nlm.nih.gov/pubmed/19376617
Image courtesy: Davita.com
Rimda Wanchoo, MD
Labels:
CKD and ESRD,
topic discussions
Panel Reactive Antibody? how do you calculate?
We always talk about the PRA is 0% and 50% and so forth. How is that calculated?
Well, there is a calculator. The CPRA estimates the percentage of donors that would be incompatible with the candidate, based on the candidate's unacceptable antigens.
Check out http://www.unos.org/resources/frm_cpra_calculator.asp
When you go to the calculator, you enter all the unacceptable antigens for the patient and it spits out a value.
Well, there is a calculator. The CPRA estimates the percentage of donors that would be incompatible with the candidate, based on the candidate's unacceptable antigens.
Check out http://www.unos.org/resources/frm_cpra_calculator.asp
When you go to the calculator, you enter all the unacceptable antigens for the patient and it spits out a value.
This has been validated by OPTN/UNOS Histocompatibility subcommittee. Then based on the center, the decision is made. This algorithm is a more accurate measure of sensitization because it accounts for both Class I and II antigens
You can learn more about it at the UNOS website
Topic Discussion: MYH9 Nephropathies
A recent review in CJASN discusses the concept of MYH9 Nephropathies. In the African American population, we have always observed many kidney diseases. Research at Wake Forrest Medical Center has revealed some excellent genetic findings. Polymorphisms in the non muscle myosin heavy chain 9 gene (MYH9) has been associated with many non diabetic kidney diseases seen in African and European derived american populations. Turns out that 45% of the ESRD groups in the African Americans have this risk variant.
There must be a second hit to take this disease to occur. What is proposed in the summary is that perhaps:
there is the first hit, the RISK, then there is this second hit: either gene interaction, environmental factors such as a virus like HIV --> then leading to kidney disease and severe hypertension. The pathology spectrum is collapsing FSGS, FSGS and focal global sclerosis.
Have a look at the summary.
http://www.ncbi.nlm.nih.gov/pubmed/20299374
Other references
http://www.ncbi.nlm.nih.gov/pubmed/20532800
http://www.ncbi.nlm.nih.gov/pubmed/20523037
http://www.ncbi.nlm.nih.gov/pubmed/20492585
There must be a second hit to take this disease to occur. What is proposed in the summary is that perhaps:
there is the first hit, the RISK, then there is this second hit: either gene interaction, environmental factors such as a virus like HIV --> then leading to kidney disease and severe hypertension. The pathology spectrum is collapsing FSGS, FSGS and focal global sclerosis.
Have a look at the summary.
http://www.ncbi.nlm.nih.gov/pubmed/20299374
Other references
http://www.ncbi.nlm.nih.gov/pubmed/20532800
http://www.ncbi.nlm.nih.gov/pubmed/20523037
http://www.ncbi.nlm.nih.gov/pubmed/20492585
Pediatrics Grand rounds continue
 The pediatric nephrology blog periodically places grand rounds that reviews news on nephrology and e-nephrology around the world. Have a look
The pediatric nephrology blog periodically places grand rounds that reviews news on nephrology and e-nephrology around the world. Have a lookhttps://www.pediatric-nephrology.com/home/2010/06/16/221-pgrix.html
CLINICAL CASE 18, ANSWER and SUMMARY
Which of the following is a known cause of granulomatous interstitial nephritis?
Sarcoidosis | 3 (37%) |
Fungal | 0 (0%) |
BCG vaccination | 0 (0%) |
Heroin abuse | 1 (12%) |
Atheroembolic Disease | 0 (0%) |
All of the Above | 4 (50%) |
None of the Above | 0 (0%) |
Most of you got this one. As we commonly associated granulomatous interstitial nephritis with sarcoidosis, that is one of the correct answers but the right answer is all of the above. Drugs such as b lactam antibiotics, nsaids and diuretics have been associated with it. Wegener GN, infections such as TB, fungal and bacterial infections, BCG vaccine, jejunal ileal bypass, heroin abuse, paraproteinemias and atheroembolic(chronic) are also causes of it. Think of these causes when you see such biopsy findings.
Labels:
Clinical Case,
General Nephrology
New blogs of interest
Not really new but i just discovered these at my own institution
This might be of interest to us since they are Immunology and Urology related.
Take a look
http://feinsteininstitute.typepad.com/feinsteinweblog/
http://www.smithinstituteforurology.com/blog/
This might be of interest to us since they are Immunology and Urology related.
Take a look
http://feinsteininstitute.typepad.com/feinsteinweblog/
http://www.smithinstituteforurology.com/blog/
Thursday, June 17, 2010
Topic Discussion: Primary vs Secondary Membranous
What things on pathology can help differentiate primary from secondary membranous GN?
Usually its secondary when there are:
1. mesangial deposits along with membranous and intramembranous deposits
2. full house pattern on IF
3. tubular reticular inclusions present on EM
4. irregularity of thickness of BM
Again these are subtle findings and its all in the right clinical context.
Usually its secondary when there are:
1. mesangial deposits along with membranous and intramembranous deposits
2. full house pattern on IF
3. tubular reticular inclusions present on EM
4. irregularity of thickness of BM
Again these are subtle findings and its all in the right clinical context.
Labels:
glomerular diseases,
topic discussions
Tuesday, June 15, 2010
CLINICAL CASE 17, ANSWER AND SUMMARY
Which drink is not good for stone formers? |
Tea | 11 (40%) |
Coffee | 6 (22%) |
Both | 10 (37%) |
So based on this study, Coffee more than tea was protective.
Other studies listed below have shown that both tea and coffee can be protective.
In summary, none of those choices are correct, sorry! bad question. It should have been neither!
Labels:
Clinical Case,
General Nephrology
TOPIC DISCUSSION: Amylase in the urine?? Hmm!!
Has anyone ever used urinary amylase levels or amylase creatinine ratio as a marker of pancreatic function. Urinary amylase has been of historical interest for the diagnosis of pancreatitis and even in some cases of pancreatic transplant rejection. Some might claim that the amylase creatinine clearance ratio (ACCR) is a more sensitive index of pancreatic malfunction, then serum amylase levels.
The renal clearance of amylase is 1-3.2 ml/min and the amylase filtered through the glomerulus is not reabsorbed by the tubular epithelium. It easily passes through the glomerular filter. Ratios of urinary amylase to urinary creatinine have proved to be sensitive for pancreatitis but increases also occur in patients hospitalized for other diseases.Hence it is not as specific as the ACCR. The amylase creatinine clearance ratio obviates variability in renal function and is useful when the patient has more than one cause for a raised serum amylase.
In 1975, Warshaw and Fuller found that the renal clearance ratios of the various isoenzymes of amylase were the same and the urinary amylase molecules in patients of pancreatitis were of the same molecular weight; as the serum amylase from normal individuals, leaving only an increased renal permeability, due to enzymatic action, kinins or other vasoactive substances to explain the rise in ACCR.
While it has been claimed to rise specifically in pancreatitis, reports of its rise in febrile illnesses, diabetic ketoacidosis and in patients with burns and increase alcohol intake have been reported.
In pancreatic transplants, usually serum lipase followed by amylase is used as an early marker of rejection. A rise in blood glucose is a late indicator of pancreas allograft rejection, and signifies that more than 90% of the islet cell mass may already have been destroyed. In allografts draining into the urinary bladder, a decrease in urinary amylase excretion is perhaps the earliest metabolic marker for rejection. But, hypoamylasuria does not prove that the injury to the pancreas is immunologically mediated, so that a tissue diagnosis is still needed to clinch the diagnosis of rejection. ACCR to my knowledge has not be studied in pancreatic transplants.
Nevertheless despite a few false positives, a rise in ACCR remains a good indicator of pancreatic damage. Wherever the urine can help, we can help ;)
Caution especially of using such ratios if the renal function is abnormal!
Image source : http://www.polyenzyme.com/images/a-Amylase.jpg
References:
http://www.ncbi.nlm.nih.gov/pubmed/1117961
http://www.ncbi.nlm.nih.gov/pubmed/2452761
http://www.ncbi.nlm.nih.gov/pubmed/95609
The renal clearance of amylase is 1-3.2 ml/min and the amylase filtered through the glomerulus is not reabsorbed by the tubular epithelium. It easily passes through the glomerular filter. Ratios of urinary amylase to urinary creatinine have proved to be sensitive for pancreatitis but increases also occur in patients hospitalized for other diseases.Hence it is not as specific as the ACCR. The amylase creatinine clearance ratio obviates variability in renal function and is useful when the patient has more than one cause for a raised serum amylase.
In 1975, Warshaw and Fuller found that the renal clearance ratios of the various isoenzymes of amylase were the same and the urinary amylase molecules in patients of pancreatitis were of the same molecular weight; as the serum amylase from normal individuals, leaving only an increased renal permeability, due to enzymatic action, kinins or other vasoactive substances to explain the rise in ACCR.
While it has been claimed to rise specifically in pancreatitis, reports of its rise in febrile illnesses, diabetic ketoacidosis and in patients with burns and increase alcohol intake have been reported.
In pancreatic transplants, usually serum lipase followed by amylase is used as an early marker of rejection. A rise in blood glucose is a late indicator of pancreas allograft rejection, and signifies that more than 90% of the islet cell mass may already have been destroyed. In allografts draining into the urinary bladder, a decrease in urinary amylase excretion is perhaps the earliest metabolic marker for rejection. But, hypoamylasuria does not prove that the injury to the pancreas is immunologically mediated, so that a tissue diagnosis is still needed to clinch the diagnosis of rejection. ACCR to my knowledge has not be studied in pancreatic transplants.
Nevertheless despite a few false positives, a rise in ACCR remains a good indicator of pancreatic damage. Wherever the urine can help, we can help ;)
Caution especially of using such ratios if the renal function is abnormal!
Image source : http://www.polyenzyme.com/images/a-Amylase.jpg
References:
http://www.ncbi.nlm.nih.gov/pubmed/1117961
http://www.ncbi.nlm.nih.gov/pubmed/2452761
http://www.ncbi.nlm.nih.gov/pubmed/95609
Monday, June 14, 2010
Gurudakshina in Nephrology
A nice piece by Dr. Ajay Singh in Kidney International July 2010 Issue talks about an interesting concept and idea in the field of medicine and nephrology. It's guru dakshina or giving back to your teachers or professors or paying back for your success. It is a nice essay on Americans of Indian origin and how they have given back to their homeland India and helped people in need in a land far away. Inspiration for all of the younger nephrologists! Check it out!
Image source: http://www.iloveindia.com/indian-traditions/gifs/gurudakshina.jpg
Image source: http://www.iloveindia.com/indian-traditions/gifs/gurudakshina.jpg
Are you aware of MICA antibodies?
 Some kidney transplants fail despite good HLA matches. The main targets for antibody mediated rejection are HLA antigens. Among non-HLA antigens that can induce an antibody response, MHC class 1-related chain A (MICA) antigens appear significant enough to affect acute and chronic graft outcomes. MICA antigens are expressed on endothelial cells, dendritic cells, fibroblasts, epithelial cells but not on peripheral blood lymphocytes. As they are expressed on endothelial cells, it seems that antibodies against MICA antigens are harmful especially to vascularized allografts like renal allograft. In a landmark study (Zou et al, NEJM Sep 2007), pretransplantation MICA antibodies were found in about 11% of 1910 renal transplant recipients. It was found that recipients with pre-transplantation MICA antibodes had lower 1-year graft survival compared to those without MICA antibodies suggesting adverse role of these antibodies. However, a more recent but smaller study (Lemy et al, Transplantation, May 2010) failed to replicate same findings. In this study, MICA antibodies did not adverse affect renal allograft outcomes.
Some kidney transplants fail despite good HLA matches. The main targets for antibody mediated rejection are HLA antigens. Among non-HLA antigens that can induce an antibody response, MHC class 1-related chain A (MICA) antigens appear significant enough to affect acute and chronic graft outcomes. MICA antigens are expressed on endothelial cells, dendritic cells, fibroblasts, epithelial cells but not on peripheral blood lymphocytes. As they are expressed on endothelial cells, it seems that antibodies against MICA antigens are harmful especially to vascularized allografts like renal allograft. In a landmark study (Zou et al, NEJM Sep 2007), pretransplantation MICA antibodies were found in about 11% of 1910 renal transplant recipients. It was found that recipients with pre-transplantation MICA antibodes had lower 1-year graft survival compared to those without MICA antibodies suggesting adverse role of these antibodies. However, a more recent but smaller study (Lemy et al, Transplantation, May 2010) failed to replicate same findings. In this study, MICA antibodies did not adverse affect renal allograft outcomes.
Labels:
immunology,
kidney transplantation,
rejection
ISBP Conference Sept 2010
A conference happening in California that might be of interest to many
The International Society of Blood purification has been designed for medical personnel that are involved in the care of renal failure patients, critically ill patients and patients with congestive heart failure. The conference addresses the needs of nephrologists, critical care specialists, hospitalists and cardiologists with an interest in blood purification, dialysis, blood filtration,kidney failure and disorders involving heart and kidney dysfunction.
Please check out their website for the event details.
Image source: http://www.isbp.org/
The International Society of Blood purification has been designed for medical personnel that are involved in the care of renal failure patients, critically ill patients and patients with congestive heart failure. The conference addresses the needs of nephrologists, critical care specialists, hospitalists and cardiologists with an interest in blood purification, dialysis, blood filtration,kidney failure and disorders involving heart and kidney dysfunction.
Please check out their website for the event details.
Image source: http://www.isbp.org/
Friday, June 11, 2010
Innovative Nephrology teaching tools!
Please take some time to do this mini survey we have prepared.
http://www.surveymonkey.com/s/
http://www.surveymonkey.com/s/
Kamal Shah's Blog: An Indian CKD registry now exists
A nice post from Kamal Shah's Blog
Kamal Shah's Blog: An Indian CKD registry now exists
CLINICAL CASE 16 , ANSWER and SUMMARY
Which disease is odd one out!!
Most of you said IgM Nephropathy. That was what I was thinking as well. Why you might ask?
This is a tough question since some might even want to say LPHS as the answer since it might not be a real glomerular disease but the other three are!
There is some data that the Alport's, Thin Basement Membrane Disease and LPHS are all sort of related diseases leading to hematuria. When renal biopsy is performed, some patients have a known cause of hematuria such as IgA nephropathy or vasculitis. Such patients are considered to have secondary LPHS, while patients without signs of acquired underlying glomerular disease are considered to have primary LPHS. Renal biopsy in patients with primary LPHS shows evidence of glomerular hematuria, as manifested by red cells in the tubules. Most of the time, specimens show thin or thick glomerular basement membranes on electron microscopy, suggesting an important role for glomerular basement membrane abnormalities in the hematuria. All three of these diseases(LPHS, Alports and TBM) are related to the glomerular basement membrane.
IgM Nephropathy on the other hand is considered a minimal change variant. Usually this is a mesangial proliferative glomerulonephritis that has prominent diffuse mesangial deposits of IgM and complement, along with electron dense deposits in the mesangium. Alports, TBM and LPHS don't have deposits making it different from IgM as well. IgM does have glomerular basement membrane pathology but its due to deposits.
Groupers would group Alports, IgA Nephropathy, LPHS and TBM in one spectrum of disease; with Alports sort of being slightly different given its genetic nature.
Groupers would group Minimal Change, IgM nephropathy, C1q Nephropathy, mesangial proliferative disease and FSGS as one group as a spectrum.
While others can single each disease separately.
Eventhough I made this question up, its a bad question! but it sort of teaches us about grouping and thinking of what diagnosis to consider in certain situation and what not to consider in certain situations.
Alport's Syndrome | 0 (0%) |
IgM nephropathy | 22 (70%) |
Loin Pain Hematuria Syndrome | 9 (29%) |
Thin Basement Membrane Disease | 0 (0%) |
Most of you said IgM Nephropathy. That was what I was thinking as well. Why you might ask?
This is a tough question since some might even want to say LPHS as the answer since it might not be a real glomerular disease but the other three are!
There is some data that the Alport's, Thin Basement Membrane Disease and LPHS are all sort of related diseases leading to hematuria. When renal biopsy is performed, some patients have a known cause of hematuria such as IgA nephropathy or vasculitis. Such patients are considered to have secondary LPHS, while patients without signs of acquired underlying glomerular disease are considered to have primary LPHS. Renal biopsy in patients with primary LPHS shows evidence of glomerular hematuria, as manifested by red cells in the tubules. Most of the time, specimens show thin or thick glomerular basement membranes on electron microscopy, suggesting an important role for glomerular basement membrane abnormalities in the hematuria. All three of these diseases(LPHS, Alports and TBM) are related to the glomerular basement membrane.
IgM Nephropathy on the other hand is considered a minimal change variant. Usually this is a mesangial proliferative glomerulonephritis that has prominent diffuse mesangial deposits of IgM and complement, along with electron dense deposits in the mesangium. Alports, TBM and LPHS don't have deposits making it different from IgM as well. IgM does have glomerular basement membrane pathology but its due to deposits.
Groupers would group Alports, IgA Nephropathy, LPHS and TBM in one spectrum of disease; with Alports sort of being slightly different given its genetic nature.
Groupers would group Minimal Change, IgM nephropathy, C1q Nephropathy, mesangial proliferative disease and FSGS as one group as a spectrum.
While others can single each disease separately.
Eventhough I made this question up, its a bad question! but it sort of teaches us about grouping and thinking of what diagnosis to consider in certain situation and what not to consider in certain situations.
Labels:
Clinical Case,
glomerular diseases
IN THE NEWS- Proteinuria and Avastin
Bevacizumab Increases Risk for Severe Proteinuria in Cancer Patients, a recent paper in JASN 2010 talks about a systemic and meta analysis of this drug in prior trials. An interest to me is this field of onco-nephrology where chemotherapy agents are causing damage and we can really learn a lot from them about podocyte biology. As we all know now that anti VEGF agents like the above mention cause proteinuria via similar mechanism as seen in pre eclampsia. Its podocytopenia. This paper analyzed 16 studies of over 12,000 patients and different tumors. When avastin was added to other chemo agents, the degree of proteinuria was significantly higher. The cancer with the highest proteinuria risk was renal cell cancer. this might be because usually these individuals getting this drug already have a nephrectomy decreasing their nephron mass.
Image source: USA today
References:
Thursday, June 10, 2010
CONSULT ROUNDS: Dialysis Membrane Reactions- Type B
Lets focus on the Type B reaction. This is much less common.
Few take home points
1. Can be seen with the new cellulosic membranes
2. Usually can occur hours into dialysis, doesn't follow the Type A rule of in first 5-10 minutes
3. Can cause hypotension, SOB, back pain and sometimes anaphylaxis
4. Its a complement induced process rather than an ethylene oxide antibody reaction as in type A
5. Can lead to neutropenia
6. Eventually improves as dialysis continues
7. The syndrome is usually prevent by the reuse of the dialyzer which then will reduce the complement levels.
Few take home points
1. Can be seen with the new cellulosic membranes
2. Usually can occur hours into dialysis, doesn't follow the Type A rule of in first 5-10 minutes
3. Can cause hypotension, SOB, back pain and sometimes anaphylaxis
4. Its a complement induced process rather than an ethylene oxide antibody reaction as in type A
5. Can lead to neutropenia
6. Eventually improves as dialysis continues
7. The syndrome is usually prevent by the reuse of the dialyzer which then will reduce the complement levels.
Wednesday, June 9, 2010
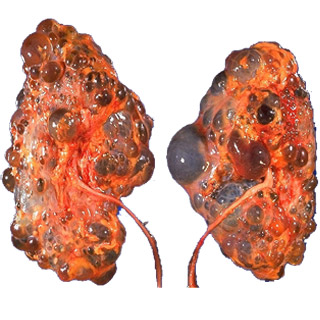
IN THE NEWS ---> New treatments for cystic disease
A new era is coming for polycystic kidney and liver disease.
Lots of studies being conducted lately, largely single centered but showing promise in the near future on two possible drugs to decrease cyst volume.
We have heard a lot about sirolimus and its effect on the cyst volume and trials showing that it will decrease cyst volume. There is data that if volume is decreased,then the progression to ESRD slows down.
Another drugs is the somatastatin analogues used in neuro endocrine tumors. Three recent trials have shown promise.
Long term data is still needed and more larger studies that are multi centered to validate data.
References:
http://www.ncbi.nlm.nih.gov/pubmed/20431041
http://www.ncbi.nlm.nih.gov/pubmed/19646443
http://www.ncbi.nlm.nih.gov/pubmed/20185596
http://www.ncbi.nlm.nih.gov/pubmed/19917358
http://www.ncbi.nlm.nih.gov/pubmed/20466742
Lots of studies being conducted lately, largely single centered but showing promise in the near future on two possible drugs to decrease cyst volume.
We have heard a lot about sirolimus and its effect on the cyst volume and trials showing that it will decrease cyst volume. There is data that if volume is decreased,then the progression to ESRD slows down.
Another drugs is the somatastatin analogues used in neuro endocrine tumors. Three recent trials have shown promise.
Long term data is still needed and more larger studies that are multi centered to validate data.
References:
http://www.ncbi.nlm.nih.gov/pubmed/20431041
http://www.ncbi.nlm.nih.gov/pubmed/19646443
http://www.ncbi.nlm.nih.gov/pubmed/20185596
http://www.ncbi.nlm.nih.gov/pubmed/19917358
http://www.ncbi.nlm.nih.gov/pubmed/20466742
Labels:
CKD and ESRD,
General Nephrology,
In The News
Tuesday, June 8, 2010
Immunology Quiz 1 Answers
Immunology Quiz Corner: Which one is Matched INCORRECTLY?
| ||||||||||
| The correct answer is Treg and IL-6. After the encounter with an antigen and co stim molecules presented by antigen presenting cells, the naive T cells that is CD4+ can differentiate into different type of T cells. The commitment to which T cell type it becomes depends on the cytokine that is pre dominant. In the presence of Interferon Gamma and IL-12, Th1 cells predominate that are responsible for intracellular bacteria and cell mediated immunity. In the presence of IL-4, Th2 dominate that are predominately for allergic diseases. In the presence of IL-6 and IL-23 in the presence of TGF-B, Th17 dominate , they are responsible for extracellular bacteria and fungi and cell mediated autoimmunity. Finally, in the presence of TGF-B and retinoic acid, FoxP3 positive T regs dominate that are regulatory in nature. There might be more regulatory T cells around in the immune system that we still haven't discovered. | ||||||||||
| A nice review of this in the context of TH17 immune response was recently published in Kidney International | ||||||||||
| http://www.ncbi.nlm.nih.gov/pubmed/20375986 |
Labels:
basic science,
immunology,
quiz
Monday, June 7, 2010
Rituximab induced lung injury
Rituximab is being used for many kidney diseases and now in the post transplant world as well
A recent report in pediatric Nephrology journal discusses a pulmonary complication of the drug.
This first report of rituximab-associated, Cryptogenic Organising Pneumonia highlights the risk of pulmonary complications after treatment with B-cell depleting agents in solid organ transplant recipients.
http://www.ncbi.nlm.nih.gov/pubmed/20140460
http://www.ncbi.nlm.nih.gov/pubmed/19681063
https://www.pediatric-nephrology.com/daily-updates/2010/05/31/212-ralimore.html
A recent report in pediatric Nephrology journal discusses a pulmonary complication of the drug.
This first report of rituximab-associated, Cryptogenic Organising Pneumonia highlights the risk of pulmonary complications after treatment with B-cell depleting agents in solid organ transplant recipients.
http://www.ncbi.nlm.nih.gov/pubmed/20140460
http://www.ncbi.nlm.nih.gov/pubmed/19681063
https://www.pediatric-nephrology.com/daily-updates/2010/05/31/212-ralimore.html
TOPIC DISCUSSION: DIABETIC NEPHROPATHY!!
This month's Nature Review Nephrology dedicated an entire journal to the Concept of Diabetic Nephropathy.
There are many articles that are in the journal but a few highlights are worth mentioning.
1. The potential role of epigenetic mechanisms in diabetic nephropathy is intriguing. Epigenetics interact with genetic information and alter genetic expression and perhaps even cause human diseases. The Epigenetics concept is growing and even human behavior can change the epigenome. These epigenomes are sort of turn on and off switches of the genes.
The mention a concept of metabolic memory of renal cells and epigenomics in diabetes is new. The question of whether transient hyperglycemia ( leading to a memory of that in the renal cells) due to glycosolated end products or AGE, can induce epigenetic modifications of gene expression by affecting the methylation of particular parts of the genome is what is discussed in one of the articles. Metobolic memory is referred to as if the cells have seen prior hyperglycemia, they keep that memory and can later on return via epigenetic mechanism to lead to diabetic disease!
2. Another article discusses the concept of nuclear hormone receptors in diabetes. Multiple nuclear hormone receptors have been linked with changes and leading to diabetic nephropahty in rat models. Some of the ones mentioned are PPARY, estrogen receptor, Vitamin D receptor, hepatocyte nuclear factor 4, farnesoid receptor, liver X receptor, and estrogen related receptors. All of these receptors in some shape of form have been linked to either renal fibrosis, proteinuria, mesangial expansion, lipid accumulation or macrophage infiltration( different stages of diabetic nephropathy)
3. The concept of RAGE or receptor of advanced glycalation endproducts is reviewed in one of the chapters.
RAGE is not only dominant player in diabetes but there have been papers regarding lupus, amyloidosis, ischemic renal injury as well. A simple way to conceptualize is the stimulus is likely elevated glucose that leads to activation of RAGE on the glomerular cells that leads to podocyte apoptosis and increase permeability; increased reactive oxygen species and increased TGF-B and fibrosis; increased CCL2 and hence increased inflammation via attraction of inflammatory cells and mesangial expansion. All these phenomenon leading to increase damage and repair leading to the pathology we see in Diabetic Nephropathy.
The references:
http://www.ncbi.nlm.nih.gov/pubmed/20421886
http://www.ncbi.nlm.nih.gov/pubmed/20421884
http://www.ncbi.nlm.nih.gov/pubmed/20421885
There are many articles that are in the journal but a few highlights are worth mentioning.
1. The potential role of epigenetic mechanisms in diabetic nephropathy is intriguing. Epigenetics interact with genetic information and alter genetic expression and perhaps even cause human diseases. The Epigenetics concept is growing and even human behavior can change the epigenome. These epigenomes are sort of turn on and off switches of the genes.
The mention a concept of metabolic memory of renal cells and epigenomics in diabetes is new. The question of whether transient hyperglycemia ( leading to a memory of that in the renal cells) due to glycosolated end products or AGE, can induce epigenetic modifications of gene expression by affecting the methylation of particular parts of the genome is what is discussed in one of the articles. Metobolic memory is referred to as if the cells have seen prior hyperglycemia, they keep that memory and can later on return via epigenetic mechanism to lead to diabetic disease!
2. Another article discusses the concept of nuclear hormone receptors in diabetes. Multiple nuclear hormone receptors have been linked with changes and leading to diabetic nephropahty in rat models. Some of the ones mentioned are PPARY, estrogen receptor, Vitamin D receptor, hepatocyte nuclear factor 4, farnesoid receptor, liver X receptor, and estrogen related receptors. All of these receptors in some shape of form have been linked to either renal fibrosis, proteinuria, mesangial expansion, lipid accumulation or macrophage infiltration( different stages of diabetic nephropathy)
3. The concept of RAGE or receptor of advanced glycalation endproducts is reviewed in one of the chapters.
RAGE is not only dominant player in diabetes but there have been papers regarding lupus, amyloidosis, ischemic renal injury as well. A simple way to conceptualize is the stimulus is likely elevated glucose that leads to activation of RAGE on the glomerular cells that leads to podocyte apoptosis and increase permeability; increased reactive oxygen species and increased TGF-B and fibrosis; increased CCL2 and hence increased inflammation via attraction of inflammatory cells and mesangial expansion. All these phenomenon leading to increase damage and repair leading to the pathology we see in Diabetic Nephropathy.
The references:
http://www.ncbi.nlm.nih.gov/pubmed/20421886
http://www.ncbi.nlm.nih.gov/pubmed/20421884
http://www.ncbi.nlm.nih.gov/pubmed/20421885
Sunday, June 6, 2010
B cell signature and Tolerance
Recently we discussed B regulatory cells. Before one could think, a study in JCI discusses this very topic of B cell signature in tolerant renal transplant recipients. This is the largest cohort of tolerant renal patients and when they did compared gene expression profiles, they found that the predominant Cell was a B cell that was regulating the maturing of most B cells. IL -10 was also significant. This B cell signature was associated with upregulation of CD20 mRNA in urine sediment cells and elevated numbers of peripheral blood naive and transitional B cells in tolerant participants compared with those receiving immunosuppression.
Finally, B cells are making a mark, just lagging slightly behind the T cells.
Hmmm. is Rituximab all good then???
Reference
http://www.ncbi.nlm.nih.gov/pubmed/20501946
http://www.ncbi.nlm.nih.gov/pubmed/20501943
Finally, B cells are making a mark, just lagging slightly behind the T cells.
Hmmm. is Rituximab all good then???
Reference
http://www.ncbi.nlm.nih.gov/pubmed/20501946
http://www.ncbi.nlm.nih.gov/pubmed/20501943
Friday, June 4, 2010
Thursday, June 3, 2010
Kidney Transplant as an Outpatient Procedure
This ATC 2010, North Shore/LIJ Center of Kidney Transplantation presented an abstract about a 48 hour discharge kidney transplant program. A nice editorial on this can be seen in the most recent ASN Kidney News. Selected patients with the right multi-team approach along with Nephrologists, Social workers and coordinators, this is very possible.
The re admission rate was low, complications were low along with a cost effective strategy.
Check it out at ASN Kidney News online version.
The re admission rate was low, complications were low along with a cost effective strategy.
Check it out at ASN Kidney News online version.
Labels:
clinical science,
kidney transplantation,
surgery
IN THE NEWS ---> Detective Nephron strikes again!
The latest issue of ASN Kidney News continues on the exiting adventures of Detective Nephron and LO Henle on a tough case again.
Its a different type of teaching tool using creative writing in a funny manner to teach a certain point in nephrology.
Any advice is appreciated to improve it and cases are welcomed as well.
Its a different type of teaching tool using creative writing in a funny manner to teach a certain point in nephrology.
Any advice is appreciated to improve it and cases are welcomed as well.
Labels:
Detective Nephron,
E-Nephrology,
In The News
IN THE NEWS --->NephrologyonDemand
Check out Dr.Tejas Desai ECU Teaching Website featured in ASN Kidney news June 2010 edition
A great resource for all nephrologist
www.nephrologyondemand.org
A great resource for all nephrologist
www.nephrologyondemand.org
Wednesday, June 2, 2010
CONSULT ROUNDS: ANURIC RENAL FAILURE
Lets go through the differential of ANURIC acute renal failure
1. Obstruction
2. Obstruction
3. Obstruction
4. ATN with severe sepsis, on pressors and multiple organ dysfunction
5. Cortical necrosis
6. Bilateral renal vein thrombosis
7. Insitu renal vein obstruction sometimes seen in the elderly following major surgery
Other causes people can think of, chime in!
1. Obstruction
2. Obstruction
3. Obstruction
4. ATN with severe sepsis, on pressors and multiple organ dysfunction
5. Cortical necrosis
6. Bilateral renal vein thrombosis
7. Insitu renal vein obstruction sometimes seen in the elderly following major surgery
Other causes people can think of, chime in!
Labels:
Consult Rounds,
General Nephrology
CONSULT ROUNDS: Hydronephrosis without evidence on imaging
When we see hydronephrosis, we associate an imaging finding with it.
Clinically, we know that it can present with anuria/oliguria, sudden onset of renal failure in the right context, hyperkalemia and hyponatremia.
There are clinical situations that can lead to a hydronephrosis that might not be apparent on imaging due to the mass effect from underlying disease state not letting any room for the kidney to expand.
1. Retroperitoneal Fibrosis
2. Cervical Cancer( classically described)
3. Any cancer with RP mets and severe carcinamatosis and mass effect.
Anyone else can think of other causes, chime in!
Labels:
Consult Rounds,
General Nephrology
Journal Club: B regulatory cells
Today at Immunology Journal Club, we discussed an article from PNAS. It was a discussion of how Apoptotic cells in the setting of BALB/C, NOD and CIA mice models, showed increased CD4+ T cell production producing IL-10 via a B regulatory cell crosstalk also producing IL-10.
This is a fascinating paper and adds to the ongoing papers on B regulatory cells. We know a lot about T regs and its relation to Foxp3 and being the "policemen" cells and causing negative regulation of immunity. B cells were classically thought of as effector cells and now there is emerging data in the last decade that there might be some role of B cells in regulation as well in Encephalitis models, Diabetes, Collagen induced arthritis and latest off the press also in murine lupus models.
This might implications once we see some human data, so far none in nephrology and transplantation, oncology and rheumatology.
Here are some very good references:
http://www.ncbi.nlm.nih.gov/pubmed/20368280
http://www.ncbi.nlm.nih.gov/pubmed/20368271
http://www.ncbi.nlm.nih.gov/pubmed/18759928
http://www.ncbi.nlm.nih.gov/pubmed/20146707
This is a fascinating paper and adds to the ongoing papers on B regulatory cells. We know a lot about T regs and its relation to Foxp3 and being the "policemen" cells and causing negative regulation of immunity. B cells were classically thought of as effector cells and now there is emerging data in the last decade that there might be some role of B cells in regulation as well in Encephalitis models, Diabetes, Collagen induced arthritis and latest off the press also in murine lupus models.
This might implications once we see some human data, so far none in nephrology and transplantation, oncology and rheumatology.
Here are some very good references:
http://www.ncbi.nlm.nih.gov/pubmed/20368280
http://www.ncbi.nlm.nih.gov/pubmed/20368271
http://www.ncbi.nlm.nih.gov/pubmed/18759928
http://www.ncbi.nlm.nih.gov/pubmed/20146707
Tuesday, June 1, 2010
CLINICAL CASE 15 , ANSWER and SUMMARY
Point the odd one out!
I think that most of you got this one right. Yes, it is Gordon's syndrome.
Proximal RTA, Toluene Intoxication, Diarrhea and Ureteroileostomy are all associated with normal hyperchloremic anion gap met acidosis but with low serum K. Gordon's syndrome is usually associated with normal or high serum K.
Leaving Proximal RTA aside, lets discuss the other options a little.
Gordon's syndrome is also known as pseudoaldosteronism Type II. Recently defects in the WNK1 and WNK4 members of the serine threonine kinases have been identified to cause this AD disease. Normally these WNKS inhibut the thiazide sensitive Na-cl co transporter. In Gordon's syndrome, there are mutations in this kinases leading to over active channel and gain of function. This leads to excessive chloride and sodium re absorption and can lead to a low renin and low aldo- hypertension. Think of this disease as Gitelman's Syndrome with HTN. You also see though short stature, dental abnormalities, low excretion of Na and a metabolic acidosis. There is hyperkalemia and this is due to the diminished sodium delivery to the cortical collecting tubule at the ROMK. You usually treat with low salt diet and/or thiazide diuretics.
In Toluene Intoxication, one sees met acidosis, hypokalemia and this is reversible. This is due to hippuric acid and other organic acid by products of toluene and that leads to a positive urine anion gap and can mimic distal RTA. Toluene intoxication can lead to a metabolic acidosis via two mechanisms. First,
it is metabolized to hippuric acid by way of benzoic acid,both of which are found in the serum of patients who abuse toluene. If renal elimination of hippuric acid is impaired or hippuric acid production is high relative to renal clearance, the molecule builds up and can produce an anion gap metabolic acidosis. Toluene intoxication may also lead to a normal anion( mostly seen) gap acidosis by impairing renal elimination of ammonium ion, the primary carrier for excess hydrogen ions. The urine osmolar gap might be the only way one can perhaps suspect a toluene intoxication and by history of course from a true distal RTA.
Hyperchloremic acidosis is observed after ureterosigmoidostomy or ureteroileostomy. Acidosis is more common with the former procedure because of the large surface area and transit time involved in the small bowel. The presence of hyperchloremic acidosis after ureteroileostomy suggests obstruction of the conduit. Usually, most of these are with hypokalemia but if there is severe obstruction, hyperkalemia could ensue.
References
http://www.ncbi.nlm.nih.gov/pubmed/20308999
http://www.ncbi.nlm.nih.gov/pubmed/15300392
http://www.ncbi.nlm.nih.gov/pubmed/6347452
Proximal Renal Tubular Acidosis | 0 (0%) |
Gordon's Syndrome | 13 (68%) |
Toluene Intoxication | 4 (21%) |
Diarrhea | 2 (10%) |
Ureteroileostomy | 0 (0%) |
I think that most of you got this one right. Yes, it is Gordon's syndrome.
Proximal RTA, Toluene Intoxication, Diarrhea and Ureteroileostomy are all associated with normal hyperchloremic anion gap met acidosis but with low serum K. Gordon's syndrome is usually associated with normal or high serum K.
Leaving Proximal RTA aside, lets discuss the other options a little.
Gordon's syndrome is also known as pseudoaldosteronism Type II. Recently defects in the WNK1 and WNK4 members of the serine threonine kinases have been identified to cause this AD disease. Normally these WNKS inhibut the thiazide sensitive Na-cl co transporter. In Gordon's syndrome, there are mutations in this kinases leading to over active channel and gain of function. This leads to excessive chloride and sodium re absorption and can lead to a low renin and low aldo- hypertension. Think of this disease as Gitelman's Syndrome with HTN. You also see though short stature, dental abnormalities, low excretion of Na and a metabolic acidosis. There is hyperkalemia and this is due to the diminished sodium delivery to the cortical collecting tubule at the ROMK. You usually treat with low salt diet and/or thiazide diuretics.
In Toluene Intoxication, one sees met acidosis, hypokalemia and this is reversible. This is due to hippuric acid and other organic acid by products of toluene and that leads to a positive urine anion gap and can mimic distal RTA. Toluene intoxication can lead to a metabolic acidosis via two mechanisms. First,
it is metabolized to hippuric acid by way of benzoic acid,both of which are found in the serum of patients who abuse toluene. If renal elimination of hippuric acid is impaired or hippuric acid production is high relative to renal clearance, the molecule builds up and can produce an anion gap metabolic acidosis. Toluene intoxication may also lead to a normal anion( mostly seen) gap acidosis by impairing renal elimination of ammonium ion, the primary carrier for excess hydrogen ions. The urine osmolar gap might be the only way one can perhaps suspect a toluene intoxication and by history of course from a true distal RTA.
Hyperchloremic acidosis is observed after ureterosigmoidostomy or ureteroileostomy. Acidosis is more common with the former procedure because of the large surface area and transit time involved in the small bowel. The presence of hyperchloremic acidosis after ureteroileostomy suggests obstruction of the conduit. Usually, most of these are with hypokalemia but if there is severe obstruction, hyperkalemia could ensue.
References
http://www.ncbi.nlm.nih.gov/pubmed/20308999
http://www.ncbi.nlm.nih.gov/pubmed/15300392
http://www.ncbi.nlm.nih.gov/pubmed/6347452
Labels:
Clinical Case,
electrolytes,
General Nephrology
Subscribe to:
Comments (Atom)
All Posts
-
▼
2010
(461)
-
▼
June
(36)
- IN THE NEWS: Three trials SHOCK the NEPHROLOGY WORLD
- IN THE NEWS:- Angiotensin-receptor blockade and r...
- CONSULT ROUNDS: Hypocomplementemia!
- IN THE NEWS ---> Stem Cells and Kidney Damage
- Answer to Immunology Quiz 2
- Rituximab for induction?
- TOPIC DISCUSSION: Phosphorous containing foods
- Panel Reactive Antibody? how do you calculate?
- Topic Discussion: MYH9 Nephropathies
- Pediatrics Grand rounds continue
- CLINICAL CASE 18, ANSWER and SUMMARY
- New blogs of interest
- Topic Discussion: Primary vs Secondary Membranous
- CLINICAL CASE 17, ANSWER AND SUMMARY
- TOPIC DISCUSSION: Amylase in the urine?? Hmm!!
- Gurudakshina in Nephrology
- Are you aware of MICA antibodies?
- ISBP Conference Sept 2010
- Innovative Nephrology teaching tools!
- Kamal Shah's Blog: An Indian CKD registry now exists
- CLINICAL CASE 16 , ANSWER and SUMMARY
- IN THE NEWS- Proteinuria and Avastin
- CONSULT ROUNDS: Dialysis Membrane Reactions- Type B
- IN THE NEWS ---> New treatments for cystic disease
- Immunology Quiz 1 Answers
- Rituximab induced lung injury
- TOPIC DISCUSSION: DIABETIC NEPHROPATHY!!
- B cell signature and Tolerance
- Nephrology World on Intragraft gene expression
- Kidney Transplant as an Outpatient Procedure
- IN THE NEWS ---> Detective Nephron strikes again!
- IN THE NEWS --->NephrologyonDemand
- CONSULT ROUNDS: ANURIC RENAL FAILURE
- CONSULT ROUNDS: Hydronephrosis without evidence on...
- Journal Club: B regulatory cells
- CLINICAL CASE 15 , ANSWER and SUMMARY
-
▼
June
(36)