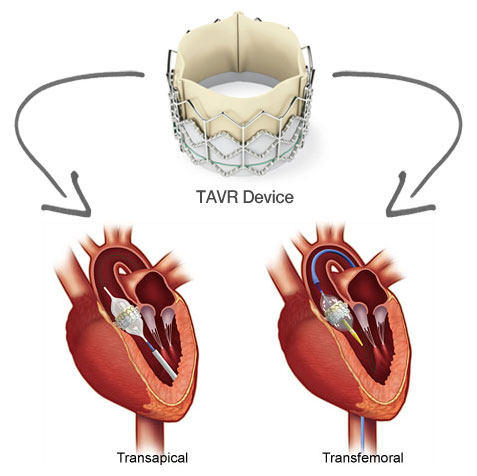
 There is increase data now that patients undergoing transcatheter aortic valve
replacement (TAVR) are at increased risk for acute kidney injury (AKI). The procedure usually involves contrast dye being used.
There is increase data now that patients undergoing transcatheter aortic valve
replacement (TAVR) are at increased risk for acute kidney injury (AKI). The procedure usually involves contrast dye being used.
Looking back to 2010, one of the earlier
studies found that AKI occurred in 11.7% of the patients following TAVR and was
associated with a greater than four-fold increase in the risk of postoperative
mortality. Hypertension, chronic obstructive pulmonary disease, and blood
transfusion were predictive factors of AKI. In those patients with
pre-procedural CKD, TAVR was associated with a significant reduction of AKI
compared with surgical AVR. In addition, studies have shown that renal function
is a predictor of mortality post TAVR.
An Italian registry abstract found similar
results. Females and patients receiving >3
RBCS units after the TAVR where more likely to develop AKI. Another
study done in 2010 published in NDT showed that transapical access, number of blood transfusions, post-interventional
thrombocytopenia and severe inflammatory response syndrome (SIRS) were risk
factors for AKI post TAVR.
The Valve Academic Research Consortium (VARC)
recently published criteria for AKI after TAVR. The main findings of the
another study indicate that AKI after TAVR is a frequent
complication, which occurs in >10% of patients. These patients have
significantly worse outcome. In agreement with previous studies, they found that the transapical approach was
associated with an increased risk for AKI. A probable explanation for this
observation may be associated with patient selection. Usually patients with
high vascular burden of disease are selected for the transapical approach and
risk of embolization post TAVR leading to AKI might be higher. Another interesting risk factor is blood
transfusion. A similar association was also identified in patients undergoing
cardiac surgery. PRBCS transfusion might
serve as a surrogate for hypotension and bleeding
or it might lead to a pro inflammatory state peri-op leading to free
iron and hemoglobin.
A
more recent analysis by Columbia University Medical Center found that
peri-procedural life-threatening bleeding was the strongest predictor of AKI after TAVR;
high white count and low platelets were also noted in the AKI group. Finally, another abstract found that male gender and
urgent need for TAVR was associated with more risk of AKI.
So in summary, what I could come up with that are risk factors
for AKI post TAVR that are fairly common in
most studies
Contrast use( debatable) as might be the
most obvious
Transapical approach
Number of Blood transfusion peri
procedure( Bleeding related), the more- the higher risk?
Post intervention thrombocytopenia
Urgent need for
TAVR

No comments:
Post a Comment