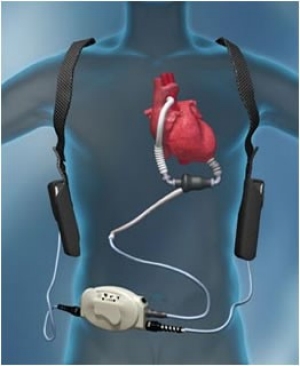
 Left ventricular assist devices (LVADs) are used increasingly as a bridge to transplantation or as
destination therapy in end-stage heart failure patients who do not respond to optimal medical
therapy. Many of these patients have end-organ dysfunction, including advanced kidney dysfunction,
before and after LVAD implantation. Kidney dysfunction is a marker of adverse outcomes,
such as increased morbidity and mortality.The incidence of AKI after LVAD implantation varies considerably: between 4 and 38 %.
Left ventricular assist devices (LVADs) are used increasingly as a bridge to transplantation or as
destination therapy in end-stage heart failure patients who do not respond to optimal medical
therapy. Many of these patients have end-organ dysfunction, including advanced kidney dysfunction,
before and after LVAD implantation. Kidney dysfunction is a marker of adverse outcomes,
such as increased morbidity and mortality.The incidence of AKI after LVAD implantation varies considerably: between 4 and 38 %. Risk factors:
INTERMACS score 1 or 2 ( http://content.onlinejacc.org/article.aspx?articleid=1143100)
Kidney <10 cm in size
Older age
ACE-I or ARB therapy immediately prior to surgery
High central venous pressure
Low LV end-diastolic dimensions
Long CPB time
Higher intraop bleeding
Need for re operation
Sepsis
Liver dysfunction
Need for blood transfusions
RV failure
CKD
Factors such as acute blood loss, volume shifts, arrhythmias, and the effect of multiple vasoactive medications influence renal hemodynamics. The sudden change in renal blood flow characteristics due to continuous flow-LVAD support can lead to AKI. Patients with preoperative RV failure and patients with INTERMACS scores of 1 or 2 are at higher risk of AKI. The RV function is of vital importance after LVAD placement since postoperative RV failure and idioventricular arrhythmias have been associated with AKI . An RV dysfunction can result in a reduced LV preload, low LVAD speeds, reduced forward flow, increased arrhythmias, and liver as well as kidney congestion.
It appears that the cause is hemodynamic vs ATN. No study has really defined the mechanism. Given the LVAD devices have pro thrombotic risk , renal vascular thrombosis and or anticoagulation related AKI should be in the differential. As always, AIN from any medication is to be considered. Hemolysis related injury could be leading to pigment nephropathy as well.
https://www.ncbi.nlm.nih.gov/pubmed/25759700
https://www.ncbi.nlm.nih.gov/pubmed/25796403

No comments:
Post a Comment