Pages
▼
Take a look here
▼
Wednesday, October 16, 2019
Saturday, October 12, 2019
Topic Discussion: HSCT associated TMA, a renal endothelial variant of GVHD
Kidney injury post HSCT is a mystery. While the initial AKI
is from multiple causes, the chronic damage we see in the survivors of HSCT is not well
understood. In a recent
review in AJKD, we did consider this to be mostly TMA related. But is TMA a
form of GVHD ( renal limited) is what some including us have proposed. When one looks at the literature
from GVHD and links to the kidney- one thinks of secondary membranous, but
perhaps this is a rare finding- endothelial glomerular damage might be more
common(TMA).
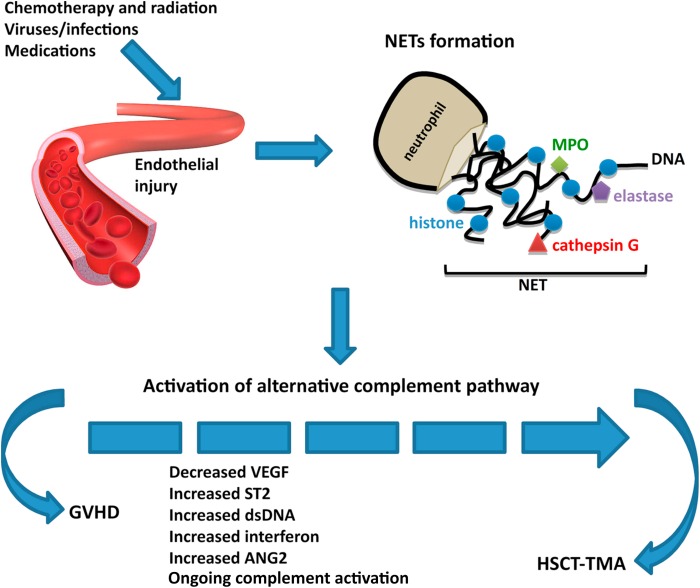
In a recent mice
study, the authors looked at HSCT effect on kidney in various murine models of
GVHD. The most common finding was glomerular with classic mesangiolysis, mesangial
proliferation and edema with subendothelial widening and microthombi. These are
features of HSCT- associated TMA. So, it is very possible that getting a HSCT
might be a second hit to several folks who might carry a complement deficiency
and perhaps there is some activation of complement system.
Some
of the literature proposes that TMA and GVHD are not related but both affect
the complement cascade. As clinicians we have seen several cases of TMA and
concurrent GVHD and a recent reported case series confirms this. It is
intriguing and possible that renal-limited TMA might be a variant of GVHD. GVHD is usually an epithelial cell disease but
having an “endothelial” target might be possible in the kidney. In most cases,
when TMA is diagnosed in a patient with HSCT, the knee jerk response is to
discontinue CNIs. Whether this is of potential benefit or harm is not clear.