FSGS is a tough diagnosis and often confusing to the
Nephrologist. Classifications in FSGS also have been very confusing and challenging. Several years ago, the pathology based classification had entered all textbooks.
Is this classification clinically useful? Not sure it is to most nephrologists? If I have a tip variant FSGS, or Perihilar, does it tell me anything re the cause and outcome? Maybe- but mostly not.
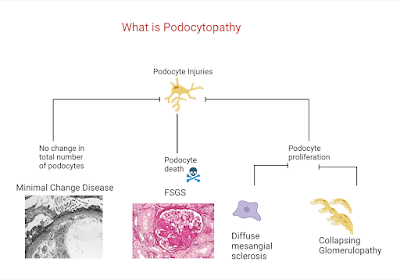
In 2007, there was a movement towards changing the concept to more podocytopathy based. ( see below- recreated using biorender).
Not sure if this is useful either but it really asked a fundamental question re how we are seeing these spectrum of diseases we term FSGS.
The most useful to me personally is classifying the FSGS presentation into
1) primary vs secondary cause
2) nephrotic syndrome vs nephrotic range proteinuria
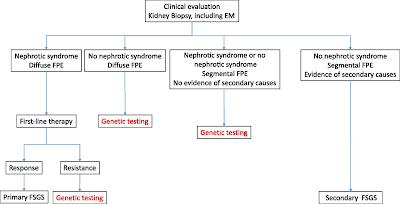
While not 100% in most cases, nephrotic syndrome and FSGS usually is going to have a primary cause( sparing some genetic causes and viruses). In addition, what is also helpful from a pathology standpoint is not the LM, but the EM--
3) Is there diffuse or partial foot process effacement?- Usually the former responds to treatment better with steroids or other immunosuppression and later is more likely a secondary cause. It may also aid in looking for a secondary cause.
This figure from a JASN paper by De Vriese et al is very helpful indeed.
So FSGS really should be described more in terms of primary vs secondary causes and EM findings to help in treatment decisions. Classically, your "permeability or immune mediated" FSGS should respond to treatment and would fit under nephrotic syndrome, diffuse foot process effacement and classically your primary FSGS. Secondary FSGS from various causes like low nephron mass, obesity, viral , meds- all classically would have nephrotic range proteinuria and sporadic foot process effacement on EM. That being said, some genetic causes of FSGS would be seen to have diffuse foot process effacement as well. Genetic FSGS is an important one to keep in mind and screening for genetic causes should be done: young patient, family hx, resistant to treatment, aiding in post transplant risk. etc.
KDIGO GN 2021 guidelines summarize this nicely
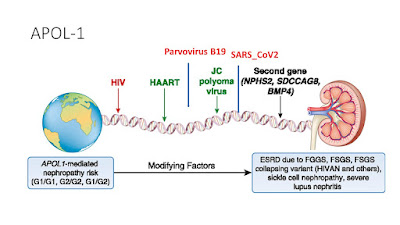
APOL-1 plays an important cause and role here and this slide can summarize the primary and the second hit concept with APOL-1 related FSGS
We should not forget --nonspecific scarring on renal biopsies. FSGS should also be differentiated from focal segmental
scarring that develops in immune-mediated GN (e.g., Membranous Nephropathy, IgA
Neph, ANCA-associated GN, and lupus nephritis) as a result of post-inflammatory
scarring of necrotizing or proliferative lesions. This happens a lot and this should not be treated as FSGS.
In summary, FSGS has come a long way and finally we are seeing some changes in the way we are describing it.. Best 3 ways to categorize FSGS is clinically and EM based.
1. Primary vs Secondary
2. Nephrotic syndrome vs nephrotic range proteinuria
3. Diffuse foot process effacement vs partial foot process effacement