Thrombotic Microangiopathy- what’s in a name?
This is a common conversation:
“ The kidney biopsy confirms TMA”. Great- we should ask hematology to help
treat..
Hematology—“ but there are no signs of microangiopathic hemolytic anemia.. no schistocytes
on smear—no need to treat”
Another conversation
“ The kidney biopsy confirms TMA”. But there are no micro thrombi on the kidney biopsy.
This is likely from HTN—treat the HTN. “
but the patient has a complement factor H mutation..”.. hmm..
The presentation of TMA can be as mild as HTN only, or AKI
on CKD or HTN with CKD or nephritic syndrome or nephrotic syndrome or just
nephrotic range proteinuria with AKI. The clinical presentation is very varied.
I have seen it all.
The problem with TMA starts with the nomenclature. Personally, I have a problem with a series of
diseases in the kidney called TMA—some have angiopathy only, some have
endotheliosis, some have both and some have additional microthrombi but at the
end we call all of them TMA.
Most of TMA cases are without thrombosis, only rarely would
you see true thrombi. Frank thrombosis
is more common in (catastrophic) APLAS associated TMA in the kidney.
Some TMA tends to be more glomerular classically in pregnancy related, for example,
with endothelial cell swelling = endotheliosis). And some TMA tends to be more arterial
(thrombotic angiopathy rather than microangiopathy). Or we might be
catching them at various points in time. A continuous process..
The pathology is also variable and hence should be considered to be defined perhaps with what is noted on it.
Endothelial injury with angiopathy
Endothelial injury with micro thrombi
Endothelial injury with endotheliosis predominant
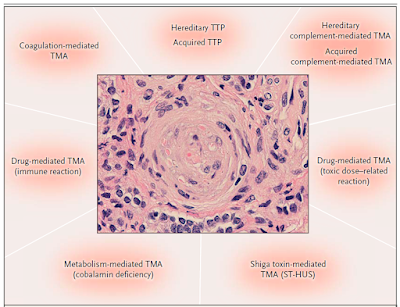
The cause of the injury than can be defined better based on
history of the patient and then divided into categories as per the syndromes of
TMA or better called “endothelial injury”- such as ADAMTS13 mediated, complement
mediated, Drug induced ( immune vs toxic), Shiga toxin mediated, metabolism
mediated, coagulation mediated and so forth. This figure is from the classic NEJM article by George et al in 2014.
As we learn more about renal endothelial injury, perhaps a better practical terminology may be useful in defining the disease to help clinicians guide the treatment plan.

nice post
ReplyDelete